Oral cancer is a serious health issue, yet many people don’t...
Read More- Home
- Services
Comprehensive Cancer Care in Mumbai
Dr. Nikhil Mitkar is committed to providing exceptional personalized cancer care services. The specialist uses modern techniques and technologies including surgery, chemotherapy, and radiation therapy when diagnosing or treating patients to achieve the desired results after these procedures have taken place. His main aim is not just treatment but also improving the life conditions of survivors among other things.
Book Your Consultation
Our team is here to give you specialized care and encouragement that will suit your needs
Services Offered by Dr. Nikhil
We offer comprehensive cancer care including expert diagnosis advanced surgical interventions and individualized recovery plans tailored to achieve the best outcomes for our patients.
- Physical Rehabilitation
- Nutritional Support
- Prosthetic Rehabilitation
- Emotional and Psychological Support
- Pain Management
- Speech and Language Rehabilitation
- Long-Term Follow-Up
- Multidisciplinary Care
- Surgical Management of Cancer
Physical rehabilitation is vital for recovery after extensive surgery, especially in restoring muscle strength and mobility. The process typically involves targeted voice therapy, swallowing techniques, and physiotherapy, all aimed at helping patients regain their physical abilities.
Voice Therapy: Post-surgery, particularly in cases involving the head, neck, or throat, voice therapy is essential to restore vocal function. Speech-language pathologists guide patients through exercises that strengthen the vocal cords, improve breath control, and enhance speech clarity, allowing effective communication.
Swallowing Techniques: Surgery can lead to swallowing difficulties, known as dysphagia, which may result in malnutrition or other complications. Rehabilitation includes specialized exercises to strengthen the swallowing muscles and improve coordination, reducing the risk of aspiration and promoting safe eating.
Physiotherapy: Physiotherapy focuses on improving mobility, flexibility, and muscle strength through personalized exercises. Physiotherapists create tailored rehabilitation plans that address the specific needs of the patient, considering the type of surgery and overall physical condition. These exercises are crucial for regaining independence and improving the quality of life.
Physical rehabilitation involves collaboration among various healthcare professionals to address the unique challenges faced by each patient. Through targeted interventions, patients can achieve significant improvements in strength, mobility, and overall well-being, enabling them to return to daily activities with greater confidence.
Nutritional support is crucial for recovery after extensive surgery, playing a key role in healing, maintaining energy levels, and supporting the immune system. In some cases, temporary tube feeding may be necessary to ensure patients receive the nutrients they need during the recovery period.
Importance of Nutrition: Post-surgery, the body’s nutritional needs increase as it works to heal. Adequate protein intake is essential for tissue repair, while vitamins and minerals support wound healing and immune function. Without proper nutritional support, recovery may be delayed, and the risk of complications can increase.
Professional Nutritional Guidance: A registered dietitian can provide personalized advice to meet increased nutritional needs. This may include high-protein foods, supplements, and hydration strategies. For patients unable to eat normally, alternative feeding methods, like tube feeding, ensure they receive the necessary nutrients.
Temporary Tube Feeding: For patients with swallowing difficulties or reduced appetite, temporary tube feeding delivers nutrient-rich liquid formulas directly to the stomach or small intestine. This ensures that the body receives the essential nutrients needed for recovery until normal eating can resume.
Ongoing monitoring and adjustments by healthcare professionals are crucial to maintaining nutritional status and supporting the healing process. By addressing nutritional needs, patients can recover more effectively, regain strength, and improve their overall well-being.
Prosthetic rehabilitation focuses on restoring function and appearance after surgery, particularly involving the mouth or face. This specialized area of recovery often includes replacing teeth with custom-made dental prosthetics that closely resemble natural teeth, as well as other facial prosthetics.
Custom-Made Dental Prosthetics: Patients who have lost teeth due to surgery, trauma, or disease benefit from custom-made dental prosthetics, such as dentures, bridges, or implants. These prosthetics are designed to match the patient’s natural teeth in color, shape, and size, ensuring a seamless and aesthetically pleasing appearance.
Facial Prosthetics: For patients who have lost or altered facial structures, custom-designed facial prosthetics restore appearance and function. These prosthetics are tailored to match skin tone and facial features, providing a natural look. Collaboration between prosthodontists, surgeons, and anaplastologists ensures that the prosthetic not only restores appearance but also supports the affected area’s function.
Rehabilitation Process: Prosthetic rehabilitation begins with a thorough assessment of the patient’s needs, followed by creating and fitting custom prosthetics. The process involves multiple healthcare professionals, including prosthodontists and surgeons, who work together to ensure optimal outcomes.
Long-term care and regular follow-up are essential to maintaining the prosthetics’ effectiveness and longevity. Patients receive guidance on proper care, ensuring their prosthetics remain in good condition and continue to support their quality of life.
Emotional and psychological support is a critical component of recovery for patients undergoing extensive surgery, particularly those facing cancer treatment. The emotional toll of surgery, combined with the stress of a serious diagnosis, can be overwhelming. Counseling sessions organized by cancer rehabilitation groups offer essential support to help patients cope with these challenges.
The Role of Counseling: Counseling provides a safe space for patients to express their fears, anxieties, and emotions related to their illness and treatment. Trained therapists or counselors lead these sessions, offering guidance, support, and coping strategies. Patients learn how to manage the emotional impact of their diagnosis and treatment, which is crucial for maintaining mental health and resilience during the recovery process.
Group Therapy and Peer Support: Many rehabilitation programs include group therapy sessions, where patients can connect with others who are going through similar experiences. This peer support is invaluable, as it helps patients feel less isolated and more understood. Sharing experiences with others in similar situations can provide comfort, reduce anxiety, and foster a sense of community.
Coping with Emotional Challenges: Patients may face various emotional challenges, including fear of recurrence, anxiety about the future, and depression related to changes in body image or physical abilities. Counseling can help patients develop effective coping mechanisms, such as relaxation techniques, mindfulness practices, and cognitive-behavioral strategies, to manage these emotions and improve their overall well-being.
In conclusion, emotional and psychological support is essential for helping patients navigate the emotional challenges associated with extensive surgery and cancer treatment. Through counseling and peer support, patients can build resilience, enhance their mental health, and improve their quality of life during recovery.
Pain management is a vital aspect of postoperative care, particularly after extensive surgery. Effective pain control is essential not only for patient comfort but also for promoting healing and recovery. Personalized pain management plans, which may include medications and physical therapy measures, are designed to address each patient’s unique needs.
Personalized Pain Management Plans: After surgery, pain levels and types can vary widely among patients. Therefore, pain management plans must be tailored to each individual, taking into account factors such as the type of surgery, the patient’s medical history, and their pain tolerance. These plans often involve a combination of medications, including opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and local anesthetics, to provide comprehensive pain relief.
Role of Physical Therapy in Pain Management: In addition to medication, physical therapy plays a crucial role in managing postoperative pain. Therapists use techniques such as massage, heat and cold therapy, and gentle exercises to reduce pain and inflammation. These methods help improve circulation, promote healing, and prevent stiffness, which can exacerbate pain. Physical therapy also empowers patients to regain mobility and strength, which can reduce the long-term effects of pain.
Monitoring and Adjusting Pain Management: Pain management is not static; it requires ongoing monitoring and adjustment based on the patient’s progress and changing needs. Regular assessments by healthcare providers ensure that pain is effectively controlled, and any side effects of medications are managed. This dynamic approach helps prevent chronic pain conditions and supports a smoother recovery.
In summary, effective pain management is critical for recovery after extensive surgery. By combining personalized medication plans with physical therapy, healthcare providers can help patients manage pain, promote healing, and enhance their overall recovery experience.
Speech and language rehabilitation is essential for patients who have undergone surgery affecting their ability to speak or communicate. This type of rehabilitation focuses on helping patients regain their communication skills, which may be impaired due to surgery in the head, neck, or brain regions. Speech therapy, often combined with the use of communication aids, plays a crucial role in this process.
Speech Therapy: After surgery, patients may experience difficulties with speaking, such as slurred speech, reduced vocal strength, or complete loss of speech. Speech-language pathologists (SLPs) work with these patients to improve their speech clarity, vocal strength, and overall communication abilities. Therapy may include exercises to strengthen the muscles involved in speech, techniques to improve breath control, and strategies to enhance articulation. The goal is to restore as much natural speech as possible.
Use of Communication Aids: In cases where natural speech cannot be fully restored, communication aids become vital. These aids can range from simple tools like picture boards to advanced technology like speech-generating devices. SLPs assist patients in selecting and using these aids effectively, ensuring they can communicate their needs, thoughts, and emotions despite their limitations.
Rehabilitation Process: The process of speech and language rehabilitation begins with a comprehensive assessment of the patient’s abilities and challenges. Based on this assessment, a personalized therapy plan is developed, focusing on the patient’s specific goals and needs. Regular sessions with an SLP, combined with at-home practice, help patients make steady progress in regaining their communication skills.
In conclusion, speech and language rehabilitation is a critical component of recovery for patients affected by surgery-related communication impairments. Through targeted therapy and the use of communication aids, patients can regain their ability to communicate effectively, improving their quality of life.
Long-term follow-up is a crucial aspect of postoperative care, especially after extensive surgery. It involves regular check-ups, monitoring of progress, and guidance on maintaining a healthy lifestyle to prevent future ailments. This ongoing care ensures that patients continue to recover effectively and reduce the risk of complications.
Regular Check-Ups: After surgery, regular follow-up appointments with healthcare providers are essential. These check-ups allow doctors to monitor the patient’s recovery, assess the effectiveness of treatment, and detect any potential complications early. Regular monitoring helps ensure that any issues, such as infection, delayed healing, or recurrence of the underlying condition, are addressed promptly.
Monitoring Progress: Long-term follow-up also involves tracking the patient’s progress over time. This includes evaluating physical recovery, such as mobility, strength, and pain levels, as well as emotional and psychological well-being. Healthcare providers may use various tools and assessments to measure progress and make necessary adjustments to the patient’s care plan.
Guidance on Healthy Living: As part of long-term follow-up, patients receive guidance on how to maintain a healthy lifestyle, which is crucial for preventing future health issues. This guidance may include recommendations for a balanced diet, regular exercise, stress management techniques, and avoiding harmful habits like smoking or excessive alcohol consumption. Patients are also educated on recognizing signs of potential complications and when to seek medical attention.
In summary, long-term follow-up is an integral part of ensuring a successful recovery after extensive surgery. By regularly monitoring progress and providing ongoing support, healthcare providers help patients maintain their health, prevent future issues, and improve their overall quality of life.
Multidisciplinary care is a comprehensive approach to treatment and recovery, particularly after extensive surgery. It involves the collaboration of various healthcare professionals who work together to address all aspects of a patient’s care, from diagnosis through the healing process. This team-based approach ensures that patients receive holistic and coordinated care.
Comprehensive Care Approach: In multidisciplinary care, a team of specialists, including surgeons, oncologists, physiotherapists, nutritionists, psychologists, and more, collaborate to develop a personalized treatment plan. Each specialist brings their expertise to address different aspects of the patient’s condition, ensuring that all physical, emotional, and psychological needs are met. This approach is particularly beneficial in complex cases, such as cancer treatment, where multiple facets of care are necessary.
Benefits of a Team-Based Approach: The primary benefit of multidisciplinary care is the seamless coordination of care. Patients receive treatment that is well-integrated, with each specialist working in concert with the others. This reduces the risk of conflicting treatments and ensures that the patient’s overall well-being is prioritized. Additionally, multidisciplinary care often leads to better outcomes, as the comprehensive nature of the approach allows for early detection of complications and more effective interventions.
Patient-Centered Care: Multidisciplinary care is also highly patient-centered. Patients are involved in the decision-making process, with the care team working closely with them to understand their preferences, concerns, and goals. This collaborative approach empowers patients, giving them a greater sense of control over their treatment and recovery.
In conclusion, multidisciplinary care is essential for ensuring that all aspects of a patient’s treatment and recovery are addressed. Through the collaboration of a diverse team of healthcare professionals, patients receive comprehensive, coordinated, and patient-centered care that improves outcomes and enhances their quality of life.
At Dr. Nikhil Mitkar’s practice, surgical management of cancer is a cornerstone of our comprehensive cancer care approach. We understand that each patient’s journey is unique, and our surgical strategies are meticulously tailored to meet individual needs, ensuring the best possible outcomes.
Expert Surgical Interventions
Our expert surgical team specializes in the precise removal of tumors, employing advanced techniques that minimize the impact on surrounding healthy tissue. The goal is to eliminate cancer while preserving as much normal function as possible. Depending on the type and stage of cancer, our surgical interventions range from minimally invasive procedures to complex surgeries involving multiple organs or regions.
Advanced Reconstructive Surgery
In cases where cancer surgery may alter appearance or function, our team is skilled in reconstructive techniques that help restore normalcy and improve quality of life. This may include reconstructing the head and neck, breasts, or other body parts affected by cancer surgery. Our reconstructive procedures are designed to achieve both functional and aesthetic restoration, helping patients regain confidence and resume their daily activities with as little disruption as possible.
Post-Surgical Rehabilitation
Recovery doesn’t end with surgery. We place a strong emphasis on post-operative care, which includes physical rehabilitation to improve muscle strength and mobility. Specialized therapies, such as targeted voice therapy and swallowing techniques, are provided for patients who have undergone extensive surgeries, particularly in head and neck cancer cases. Our multidisciplinary team collaborates to ensure that each patient receives comprehensive care, addressing both the physical and emotional aspects of recovery.
Book Your Consultation
Begin the healing process now. Our team is here to give you specialized care and encouragement that will suit your needs
What Our Patients Say
Life-Saving Expertise
and Care
From Misdiagnosis to Full Recovery
Compassionate Cancer Treatment Journey
Frequently Asked Questions
Common Questions About Our Cancer
He is an expert at treating head and neck cancers. He is highly skilled in surgical oncology for various cancers originating from these areas, thus providing holistic care that suits each individual patient’s needs.
You may contact our clinic via phone or email to arrange a consultation appointment today. Our team will help you find the nearest appointment slot convenient for you and guiding through any necessary preliminary information required before the visit.
The first time when you see Dr. Mitkar; he will go through your medical history files, conduct a physical examination if required as well as chat about symptoms that trouble you most among other things. Besides, he will advise on further diagnostic tests and outline customized treatment plans where applicable.
Depending on the type and stage of cancer, the treatment process may take a different length of time. Dr. Mitkar will provide you with a detailed timeline during your consultation that will include surgery duration, expected recovery period, and any supplementary treatments such as chemotherapy or radiation.
Dr. Nikhil Mitkar is a fellowship holder in Head & Neck Oncology and Reconstruction Surgery from DYPU, Mumbai, an MDS in Maxillofacial Surgery from Udaipur, as well as having completed observerships and has practical exposure to head and neck oncology and cleft lip and palate surgery.
Dr. Mitkar has treated more than 300 cancer patients successfully. With his expertise in head and neck oncology surgery, he has managed to attain high success rates by focusing on both removing cancerous cells and preserving the functionality of body organs.
Our Blogs
Stay informed with the latest dental health tips, treatment options, and clinic news through our informative blog posts.
Oral Cancer Aftercare: Your Guide to Recovery
Recovering from oral cancer treatment is a journey that requires time,...
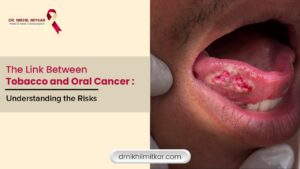
Read MoreThe Link Between Tobacco and Oral Cancer: Understanding the Risks
Tobacco use is one of the most significant and preventable causes...
Read MoreFor more information about our services or to schedule an appointment, please contact Dr. Nikhil & Our team is here to provide the best Cancer care in Mumbai.
Top Services
Quick Links
Need Support
Please explore our contact page to find relevant information and assistance.
- nikhilmitkar37@gmail.com
- +91 99304 73676
- dr_nikhil_mitkar_
- Head & Neck Cancer Clinic, 6, opposite New English School Marg, Government Colony, Bandra East, Mumbai, Maharashtra 400051